About 24 percent of U.S. adults have a liver condition that can negatively impact their health, and most don’t even know it. Fortunately, it can generally be reversed.
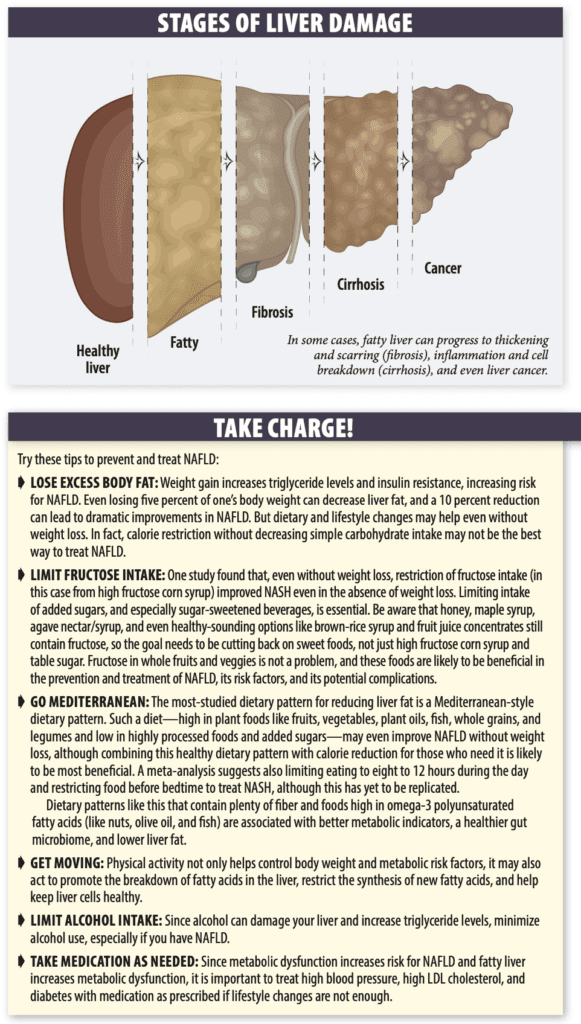
Fatty Liver. An accumulation of fat in the liver in the absence of excess alcohol intake is known as nonalcoholic fatty liver disease (NAFLD). NAFLD is the most common liver disease in the world…and prevalence continues to rise. Non-alcoholic fatty liver can lead to the development of inflammation that can progress to liver damage, liver cancer, cirrhosis, and even liver failure. This type of NAFLD is called nonalcoholic steatohepatitis (NASH). Overall, it’s estimated that three to six percent of people with fatty liver will develop NASH.
While NAFLD typically has no symptoms of its own, it is associated with type 2 diabetes and cardiovascular disease, including heart attack and stroke. In fact, the leading cause of death in patients with NAFLD is cardiovascular disease.
Who is at Risk? Researchers have identified a number of factors that likely contribute to build-up of fat in the liver, including excess body fat, genetics, the gut microbiome, and—most importantly—dietary intake.
The biggest risk factor for NAFLD is carrying excess body fat. Research suggests up to 75 percent of people who are overweight and more than 90 percent of people who have extreme obesity (BMI of 40 or over) have NAFLD. That said, it’s important to note that about 10 to 20 percent of Americans and Europeans in the “normal weight” BMI range have NAFLD.
People with NAFLD are likely to have features of metabolic dysfunction, including high body mass index (BMI), dyslipidemia (high triglycerides and LDL cholesterol and low HDL cholesterol levels), high blood pressure, high blood sugar levels, type 2 diabetes, and waist circumference over 40 inches in men and over 35 in women. These factors promote the accumulation of fat in the liver, and, conversely, fatty liver increases the risk for these metabolic disorders. This bi-directional relationship is so strong, some experts are recommending changing the official name of NAFLD to metabolic-associated fatty liver disease (MAFLD).
More than half of people with type 2 diabetes (which is a metabolic disorder) have fatty liver. Women who had gestational diabetes are also at increased risk. Insulin resistance (pre-diabetes), even without type 2 diabetes, is a risk factor as well. The more of these risk factors you have, the higher your risk of developing NASH.
Genes may play a role in who develops NAFLD. Researchers suggest this may be why risk varies by racial and ethnic groups. Individuals of Hispanic descent have the highest risk, followed by Americans of Asian descent and non-Hispanic whites. Non-Hispanic Blacks have the lowest risk of all ethnicities. While risk increases with age, even children can develop NAFLD (an estimated 10 percent of U.S. children ages two to nineteen have the condition).
The gut microbiome may also play a role in the development of NAFLD. Researchers have found differences between the bacteria that live in the digestive tracts of people with and without NAFLD. While more research is needed in humans to confirm the importance and mechanisms of this relationship, scientists theorize the compounds these bacteria make when they break down the food we eat (metabolites) may impact the liver.
Since many of these factors are impacted by diet quality, what we eat and drink is key to minimizing the development of NAFLD as well as treating it.
Diet and Fatty Liver. Overall, excess calorie intake appears to be one of the most important dietary determinants for the development of liver fat. Some specific dietary components are associated with the development of NAFLD outside of calories alone:
➧ Fat: While it is natural to think eating more fat in the diet would lead to fatty liver, this is not strictly true. Research suggests diets high in saturated fat increase liver fat content, while diets high in unsaturated fats may not, and that diets high in omega-3 unsaturated fats may reduce liver fat.
➧ Protein: “While many people think eating protein is a healthy choice, eating too much protein, without significant strength training to build muscle at the same time, contributes to the development of liver fat,” says Dariush Mozaffarian, MD, DrPH, dean of policy for the Friedman School and editor-in-chief of this newsletter. “If your muscles are not being built by training, the protein is extra calories and drives up insulin levels.”
➧ Carbohydrates: High intake of added sugars and refined grains appear to be the leading dietary driver of liver fat development. “With high intakes, the sugar molecule called fructose is metabolized in the liver to fat,” says Mozaffarian, “and the same can happen with glucose.” When the liver is overwhelmed by an influx of fructose and gut microbiota-derived fructose metabolites, fat creation (novo-lipogenesis) increases, and this new fat can accumulate in the liver.
In its natural state, fructose is found primarily in fruits and vegetables, and also honey and maple syrup. It pairs 50/50 with the sugar glucose to make sucrose (table sugar). Added sugar is primarily extracted, refined sucrose from sugar beets or sugar cane. Fructose tastes sweeter than glucose (which is why starch—100% glucose—does not taste that sweet). Regular corn syrup has less fructose (and is less sweet) than table sugar, while “high fructose” corn syrup has added fructose to make it more similar to sucrose (for example, either 58 percent glucose/42 percent fructose or 45 percent glucose/55 percent fructose). Agave nectar is approximately 80 percent fructose.
“The dose and food source of fructose really matter,” says Mozaffarian. “Research shows that fructose from whole fruit or other whole foods is at a low dose, slowly digested, and does not lead to fatty liver. High doses of this sugar or refined grains that are digested quickly—such as from sugar-sweetened beverages or table sugar—are the problem.”
Intake of highly processed foods and beverages are the leading contributor of added sugars in the U.S. A prospective study involving over 16,000 participants in China reported an association of added sugar intake with higher risk of NAFLD. Another study from China found dietary patterns rich in animal foods or sugar were associated with higher risk of NAFLD, but vegetable-rich dietary intake was not.
What to Do. Lifestyle plays an important role in the prevention and treatment of NAFLD. In fact, a heart-healthy dietary pattern and regular physical activity are the primary intervention for NAFLD, including NASH. The goal is to lose as much excess body fat as possible and control blood sugar, blood pressure, and blood triglyceride and cholesterol levels. The Take Charge! box lays out tips for preventing and getting rid of liver fat based on the latest research.
























The section on carbohydrates is inadequate and does a disservice to your readers. Complex carbs are wonderfully health-promoting. A distinction should be made between “simple carbs” and “complex carbs.”