Although headlines sometimes give the impression that one ground-breaking nutrition study will change food-based guidance, this is rarely, if ever, the case. Take a look at these examples of when studies were overhyped or misinterpreted—and why—so you’ll know how to make the best decisions for you and your family.
1. Animals Are Not People
In the 1970s, researchers found that very high intakes of the calorie-free sweetener
saccharin caused bladder cancer in rats. At the time, lots of people had already been using saccharin (which was discovered in the late 1800s) for a long time. Beginning in 1977, foods sweetened with saccharin had to have a cancer warning label. But in 2000, scientists discovered humans metabolize saccharin differently than rats, making the supposed cancer connection incorrect. The warning labels were removed.
What we learned: The results of animal studies should not be automatically generalized to humans. Animal research is important for addressing questions that cannot be studied in humans. Findings from animal studies may help researchers narrow down their search for answers or suggest a direction for human research, but animals are not humans.
What to do: When you read about a new nutrition breakthrough, see if the article mentions whether animal models or humans were studied.
2. The Antioxidant Explosion

Antioxidants (like vitamin E, vitamin C, beta-carotene, and lycopene) have been all the rage since the 1990s. Foods that contain them (like berries, cocoa, green tea, pomegranate juice, legumes, and many fortified processed foods), as well as supplements, love to tout their benefits on labels and in advertisements. Should you believe them? Yes, and no.
Antioxidants play an important role in the body, minimizing a normal but potentially dangerous condition called oxidative stress. In what sounds like something out of a thriller, unstable molecules called “free radicals” roam the body, stealing electrons from unsuspecting stable molecules. This can lead to cell damage that is involved in the development of atherosclerosis (hardening of the arteries), which increases risk of heart attack and stroke. Oxidative stress can also turn cells cancerous and accelerate the onset of dementia, among other things. Antioxidants counteract these free radicals.
Often, when a news article or website touts the antioxidant effects of a vitamin, mineral, or plant compound (phytochemical), those effects were observed when that isolated antioxidant was exposed to human cells or tissue in vitro (in test tubes or petri dishes). The same effect may or may not take place in the complex setting of the human body. In fact, although results have been mixed, research on antioxidant supplements involving humans has been disappointing. “One potential reason for the disappointing results is that our bodies have multiple antioxidant systems frequently working in concert,” says Alice H. Lichtenstein, DSc, Stanley N. Gershoff professor of nutrition science and policy at Tufts’ Friedman School and director of the Cardiovascular Nutrition Laboratory at the Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University. “In addition, as long as we are meeting our requirements for a nutrient with antioxidant properties through the foods we eat, there is no reason to expect more is better. In fact, some studies have identified negative effects of high dose antioxidant supplements.”
What we learned: We now know antioxidants have many functions in the body. Depending on the circumstances, compounds that act as antioxidants some of the time can act as dangerous free radicals at other times. “Dietary patterns containing foods rich in antioxidant compounds have consistently been linked to better health,” says Lichtenstein, “but we can’t say for sure these benefits are due to the antioxidants alone.”
What to do: Antioxidants occur naturally in whole foods, especially fruits, vegetables, legumes, nuts, seeds, and whole grains. The antioxidant capacity of a food does not make it necessarily healthier than another food. (For example, blueberries were found to have very high antioxidant levels, but other berries and fruits are equally good choices for overall health.) Eating a variety of plant foods is your best bet for health, rather than a whole lot of one specific food. A healthy dietary pattern is the best way to achieve an adequate intake of antioxidant nutrients—as well as fiber, vitamins, minerals, and everything else your body needs. “There are many benefits beyond antioxidants of habitually consuming a healthy dietary pattern rich in fruits and vegetables, whole grains, fish, legumes, nuts, seeds, and healthy plant oils that is low in added sugars and salt,” Lichtenstein says.
3. The “French Paradox”
An ecologic study (comparing different nations or populations) published in 1993 found people in Finland had a much higher risk of dying from coronary heart disease than people in France, even though both countries had very similar dietary cholesterol and saturated fat intakes. This became known as the “French Paradox.” Researchers then set out on a quest to determine what was different about the French. Since drinking red wine is a big part of French culture, many researchers focused on that. This single study was a driving factor behind the idea that red wine—and, by extension, the phytochemical resveratrol it contains—is good for heart health. This idea is still unproven, and human studies so far have been disappointing.
While this ecologic study opened up an interesting avenue for further study, it probably pointed people in the wrong direction. There were many other differences between Finland and France, including in other dietary habits and level of physical activity. Cohort studies are a better type of observational study, comparing people within a population and allowing careful adjustment for differences between people. One example is the coffee study mentioned in last month’s issue. Coffee was found to be associated with higher risk for cancer—until it was shown that many of the coffee drinkers in the cohort study were smokers, and it was the smoking that was causing the cancer.
What we learned: There are different types of observational studies: ecologic, case-control, and cohort. Ecologic studies, like the one that suggested the “French Paradox,” are the weakest type of evidence. Retrospective case-control studies also have key limitations. While observational studies cannot necessarily prove cause and effect, carefully adjusted cohort studies provide the strongest evidence that two things may be independently associated with each other.
What to do: Be aware that many nutrition studies are observational, and not all observational studies are created equal. Large, prospective cohort studies can provide the best evidence but, unless also supported by other types of research, may not be a sufficient reason to change dietary guidelines—or your behavior.
4. The Egg Flip
From 1961 until 2015, most major dietary recommendations in the U.S. includ
ed advice to limit intake of cholesterol from foods to 300 milligrams (mg) per day. We knew that high levels of LDL (“bad”) cholesterol in the blood increased risk for cardiovascular disease, so limiting or avoiding foods that contained cholesterol seemed logical. Foods like eggs and shrimp, which are high in cholesterol but low in saturated fat, were “off the menu” for many people.
Further assessment of the data showed that, at the levels at which we currently consume dietary cholesterol in the U.S. (about 300 mg a day), dietary cholesterol does not play a large role in controlling LDL (“bad”) cholesterol levels. “The major dietary determinant of LDL cholesterol levels is a higher ratio of dietary saturated fat to unsaturated fat,” says Lichtenstein. “There was a relationship between high intake of eggs (about five eggs per day) and LDL cholesterol levels, but intake of reasonable quantities of foods high in cholesterol but low in saturated fat (like eggs and shrimp) is no longer considered a concern.”
What we learned: Recommendations evolve as new data emerges. “You can generally rely on dietary guidelines like the Dietary Guidelines for Americans and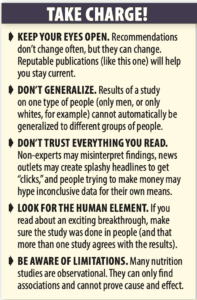 recommendations put out by public health non-profits (like the American Heart Association and American Diabetes Association), and international bodies (like the World Health Organization),” says Lichtenstein. “Groups of experts analyze all the existing research to provide strong, evidence-based information geared to be helpful to the majority of individuals.”
recommendations put out by public health non-profits (like the American Heart Association and American Diabetes Association), and international bodies (like the World Health Organization),” says Lichtenstein. “Groups of experts analyze all the existing research to provide strong, evidence-based information geared to be helpful to the majority of individuals.”
What to do: One study does not change recommendations. New data is merged with existing data, and guidance is re-assessed and potentially revised. Don’t be taken in by articles or advertisements claiming some new study is groundbreaking. Keep an eye on publications like this one to inform you of any true changes to nutrition advice.
























