You know you’re in trouble when you start seeing terms like “Syndrome X” to describe a health condition. In the late 1990s, recognition grew of a particularly potent cluster of risk factors for cardiovascular disease and diabetes. It came to be known as the metabolic syndrome.
The only visible sign of the syndrome is abdominal obesity. The other hallmarks are high triglycerides (a type of fat in the blood, or lipid), low “good” HDL cholesterol, elevated blood pressure, and high fasting blood glucose.
This cluster of risk factors is referred to as a syndrome because when they occur together they indicate a greater risk for disease than any one on its own. Having three or more of the risk factors adds up to a diagnosis of metabolic syndrome.
The precise definition of metabolic syndrome has changed over the years. But no matter how it’s diagnosed, metabolic syndrome is a pretty risky condition. “Over a period of 5 to 10 years, your chance of heart attack and stroke doubles and you are 5 times more likely to be diagnosed with diabetes,” says Jos Ordovs, PhD, director of the Nutrition and Genomics Research Lab at Tufts’ HNRCA.
Ordovs served on a panel of experts from academia, government, and industry convened by the International Life Sciences Institute to take stock of the evidence for the various steps you can take to cut your risk of metabolic syndrome. The review was published in May 2017 in Nutrition Reviews.
There is no specific medication for metabolic syndrome, although you may also end up taking drugs to address individual risk factors (triglycerides, cholesterol, or high blood pressure). Healthy lifestyle changes are essential to preventing metabolic syndrome.
“I rarely use the term metabolic syndrome with patients,” says endocrinologist Richard D. Siegel, MD, codirector of the Diabetes and Lipid Center at Tufts Medical Center. “The focus is really on improving each of these individual components, hoping that the lifestyle changes, like increasing exercise, may improve more than one risk factor.”
Lifestyle Changes: The steps you should already be taking to enhance cardiovascular fitness and general health also address metabolic syndrome.
Lose Weight: For those struggling to shrink their abdominal zone, gradual weight loss is the most successful strategy. That means a healthy eating pattern and regular exercise, rather than a rapid weight-loss push.
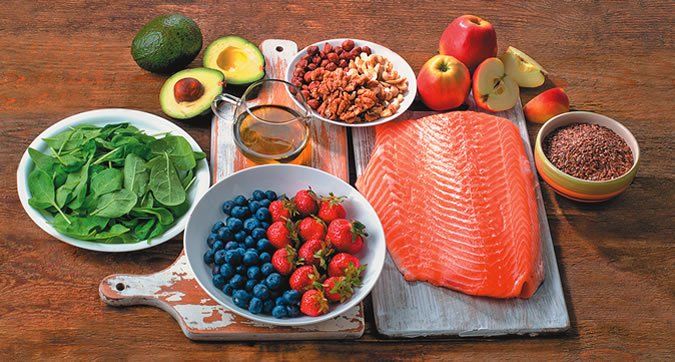
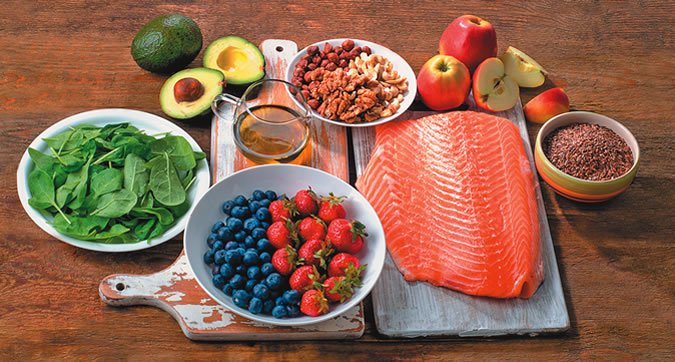
Eat Healthy Food: People who follow a healthy eating pattern are at lower risk for metabolic syndrome and a host of other health problems. The options are plentiful. For example, some research has shown that people who eat a Mediterranean dietary are at lower risk for metabolic syndrome. It’s primarily a plant-based diet, including generous portions of fruits, vegetables, whole-grain cereals, and legumes, with nuts and olive oil as the main sources of fat. It also includes fish and poultry in low-to-moderate amounts, and a relatively low amount of red meat. It’s not the only option, but it may work for you. The 2015-2020 Dietary Guidelines for Americans defines what is a healthy eating pattern for overall good health, including preventing metabolic syndrome. (See page 3, “What’s A Healthy Breakfast?” for more details.)
Exercise Regularly: Exercise is especially helpful. People who exercise regularly are at lower risk across the board for major chronic diseases, like heart disease—not just metabolic syndrome. Any physical activity is beneficial compared with none. Federal guidelines recommend 150 minutes of moderate aerobic exercise per week in increments of 10 minutes or more. Add to that resistance training two days a week to enhance muscle mass and function.
Avoid Added Sugars: Observational studies have linked excessive sugar intake to greater risk for abdominal obesity, a risk factor for metabolic syndrome. Excess sugar and calories also raise triglycerides. Cutting out sugar-sweetened drinks can significantly lower triglycerides.
Consume Alcohol in Moderation: People who drink moderate portions of alcohol are at lower risk for developing metabolic syndrome. Moderate alcohol intake means 1 to 2 drinks per day for men and 1 drink per day for women. A standard drink is 12 ounces of beer, 4 ounces of wine, 1.5 ounces of 80-proof (hard) liquor, or 1 ounce of 100-proof (hard) liquor.
However, if you do not regularly consume alcohol it is not recommended that you start drinking just to decrease your risk of developing metabolic syndrome.
The Big Picture: If you have risk factors for metabolic syndrome, don’t get too wrapped up in medical terminology. The steps you need to take are the same ones that lower the risk for heart attacks, strokes, and diabetes. “Whether someone only has central obesity and is trying to get their weight down, or has additional components of metabolic syndrome, I’m still going to be recommending all of the same good things, like a healthy diet and physical activity,” Siegel says.
Various groups of experts have come up with ways to define metabolic syndrome. They include the American Heart Association, the International Diabetes Federation, and the World Health Organization. But having three or more of the following risk factors means you have metabolic disorder:
➧ Large Waistline. This means belly fat that produces an “apple shaped” midsection, also called central or abdominal obesity. Most of the fat tissue is around the organs in your abdomen, called visceral abdominal fat. A useful rule of thumb for abdominal obesity is a waistline of 40 inches or greater in men and 35 inches or greater in women. Among Asian people, the excess internal fat may not produce the same apple‑shaped pattern seen in Caucasians.
➧ High Fasting Triglycerides. Triglycerides are a type of fat found in the blood. A triglyceride level of 150 milligrams per deciliter (mg/dL) or higher, after an overnight fast, is a risk factor. So is having to take medication to lower triglycerides. (The unit mg/dL is used to measure triglycerides, cholesterol, and blood sugar.)
➧ Low HDL Cholesterol. HDL cholesterol sometimes is called “good” cholesterol because it helps promote artery health. An HDL of less than 50 mg/dL for women and less than 40 mg/dL for men is a risk factor for metabolic syndrome. Having to take medication for low HDL cholesterol is also a risk factor.
➧ Elevated Blood Pressure. A blood pressure of 135/85 millimeters of mercury (mmHg) or higher, or being on medicine to treathigh blood pressure, is a risk factor for metabolic syndrome. If only one of your two blood pressure numbers is high, you’re still at risk.
➧ High Fasting Blood Sugar. As cells start having trouble taking up blood sugar (glucose), levels start to rise. Normal blood glucose after an overnight fast should be less than 100 mg/dL. A fasting blood sugar (glucose) of 100 mg/dL or higher, or being on medicine to treat high blood sugar, is a risk factor for metabolic syndrome. A level between 100-125 mg/dL is consideredprediabetes, and 126mg/dL or higher isdiabetes.