
How many times have you heard the message that Americans—particularly older adults—need adequate amounts of calcium and vitamin D for bone health? Major fractures of the hip or spine, often as the result of a fall, can send people to hospitals and nursing homes and raise the risk of disability and death. The Institute of Medicine (IOM) recommends daily intake of 1,000 to 1,200 milligrams (mg) of calcium and 600 to 800 international units (IU) of vitamin D, depending on age.
While eating a healthy diet rich in calcium and vitamin D is still a solid recommendation, it remains unclear who should take supplements. A recent study in the Journal of the American Medical Association addressed this question. They identified 33 clinical trials that tested whether supplements with calcium, vitamin D or both reduced the risk of fractures among community-dwelling adults aged 50 years or older. The researchers combined the results of these trials using a technique called meta-analysis.
What they found: Taking calcium and vitamin D supplements made no difference overall or in subgroups defined by calcium or vitamin D dose, gender, fracture history, dietary calcium intake, or baseline vitamin D blood levels.
Millions of adults take calcium and vitamin supplements. What should theydo?
“The key is not to have the public jumping on and off supplements every time there is a new report,” says Bess Dawson-Hughes, MD, director of Tufts’ HNRCA Bone Metabolism Laboratory. As for the new meta-analysis, she adds, “there is nothing here that in any way indicates that you should not be meeting the IOM requirements.”
It’s important to keep in mind that not all studies—and particularly meta-analysis studies—are assessing the same questions. The specific question that researchers aim to address is relevant to interpreting the conclusions.
Preventing Fractures: In the new meta-analysis, researchers identified trials that had tested the effects of calcium, vitamin D, or both, compared with taking a placebo or “dummy” pill or no treatment. The resulting 33 studies included more than 51,000 people in the US, Europe, China, Australia, and New Zealand.
Individually, the 33 trials had come to various conclusions about supplements and fractures—some positive, some negative, some neutral. Meta-analyses pool such disparate results and get an overall sense of how well a treatment works.
In this case, pooling all the trials, the dietary supplements had no significant benefits among community-based older adults. If that’s accurate, then taking calcium and vitamin D supplements does not prevent major fractures in this population.
Does Dose Matter? Dawson-Hughes explains that the findings of a meta-analysis can depend on the details of how the study is conducted. She believes this new study of fractures has some important weak spots that cast some doubt on its conclusions. Both large and small trials were part of the meta-analysis, but two of them had an outsized influence on the end results. One is the Women’s Health Initiative (WHI). Launched in 1993, the WHI enrolled more than 161,000 post-menopausal women for a series of clinical trials, including one on calcium and vitamin D for preventing fractures.
The other influential study was the Randomised Evaluation of Calcium Or vitamin D (RECORD), a trial of 5,292 people aged 70 years or older in Britain. In the meta-analysis, the WHI and RECORD trials account for 87% of the measured effect of calcium and vitamin D on hip fractures (in this case, no effect).
In the WHI, women were asked to take 400 IU of vitamin D every day. But research by Dawson-Hughes and others suggest that 400 IU is not enough to reduce hip fractures, whether by maintaining bone strength (vitamin D helps the body absorb calcium) or preventing muscle weakness that can lead to falls (and therefore fractures).
“Previous analyses of a similar nature indicate that 400 IU is not sufficient to lower fracture risk [in older adults],” Dawson-Hughes says. “You have to get up to 700 to 800 IU a day to see benefit.”
Dose is also a potential problem in the RECORD study, Dawson-Hughes says. For five years, trial participants were mailed health questionnaires and 800 IU vitamin D pills. Partway through the trial, researchers discovered that only about half of participants were adhering to the study “rules” and taking their pills. So, on average, the participants—as a group—were taking the equivalent of 400 IU of vitamin D. Again, that’s probably not enough to make a difference.
“It says that 87% of their result is based on whether a dose of 400 IU or less prevents hip fractures, and the answer is no,” Dawson-Hughes says. “I’m not surprised.”
Dawson-Hughes explains that combining the average results of multiple studies can be misleading. In this case, many participants in the studies pooled by the meta-analysis may have been taking inadequate doses of vitamin D.
Healthy or Frail – the Risk of Falls: Another relevant point may be the types of trials included in this meta-analysis: trials of adults living in the community. Some evidence suggests that vitamin D may be most useful for preventing falls (and therefore fractures) in frail elderly adults at high risk of falls, such as those in nursing homes. For example, an earlier 2014 meta-analysis by the Cochrane Collaboration included trials of vitamin D with or withoutcalcium in community, nursing home and hospital inpatient populations of postmenopausal women and older men. They concluded that vitamin Dalone is unlikely to preventfractures, but that combined supplements ofvitamin Dandcalciummay prevent hip fractures and totalfractures.
The conclusions of these two meta-analyses—and the potential relevance of risk for falls—is consistent with 2013 recommendations from the US Preventive Services Task Force (USPSTF). It determined that “current evidence is insufficient” to make any determination about the balance of benefits versus harms of combined vitamin D and calcium supplementation to prevent fractures in men or women. The USPSTF actually recommended against average doses of vitamin D and calcium supplementation to prevent fractures in postmenopausal women. The only group for whom the Task Force recommended vitamin D supplements was for older adults (age 65+) who also have any condition placing them at increased risk for falls.
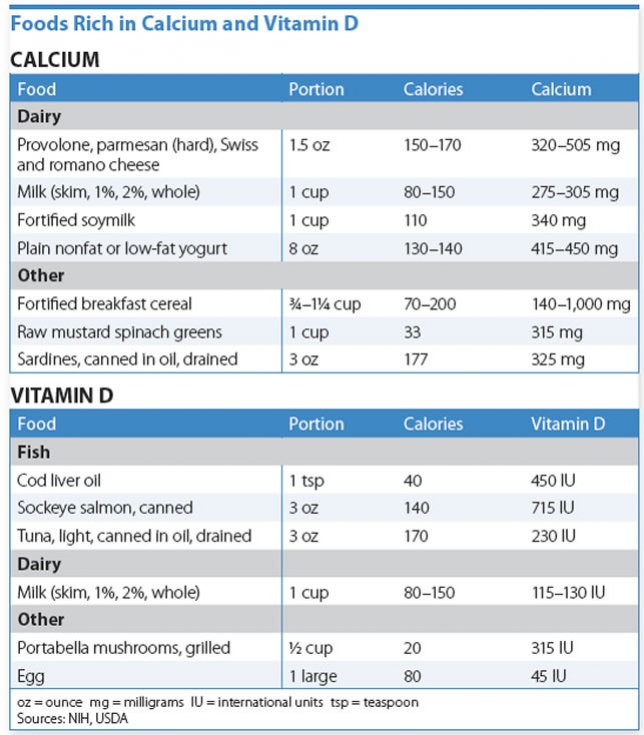
What Should You Do? The IOM guidelines set recommended dietary intakes of calcium and vitamin D for the general population to maintain health. If your levels are low, eating healthy foods is still the best route to aim for adequate calcium and vitamin D. (See “Foods Rich in Calcium and Vitamin D.”)
There is a blood test to measure vitamin D levels in the blood, but guidelines do not recommend routine testing for everyone.
“When you go to your doctor once a year for a checkup, and you are 50, 60 or 70 and healthy and getting outside, do you need your vitamin D checked? No,” Dawson-Hughes says.
However, people with risk factors for vitamin D deficiency could benefit from testing, Dawson-Hughes says. Those risk factors include obesity (body mass index [BMI] of 25 or higher); darker skin; known osteoporosis (low bone density); and difficulty absorbing calcium or vitamin D.
People at risk of serious deficiencies, and also older adults at risk for falls, have bones that are more likely to fracture, so they need advice on supplements from their doctors, tailored to their individual status and risk factors. For the rest of us, eating a healthy diet is still a great recommendation, and talk to your doctor if you think further supplements are needed.
Here are weight-bearing and muscle-strengthening exercises recommended to support bone health:
-Weight Bearing/Low Impact: Using elliptical training machines. Doing low-impact aerobics. Using stair-step machines. Fast walking on a treadmill or outdoors.
-Weight Bearing/High Impact: Dancing. Doing high-impact aerobics. Hiking. Jogging/running. Jumping rope. Stair climbing. Tennis.
-Muscle Strengthening: Lifting weights. Using elastic exercise bands. Using weight machines. Lifting your own body weight. Standing and rising up on your toes.
Source: National Osteoporosis Foundation<www.nof.org>
























