Good nutrition is important at every stage of life, and when a woman is eating for two, food decisions can be even more confusing and stressful! If you or someone in your life is pregnant or hoping to become pregnant, there are a few key dietary needs to keep in mind. To celebrate the mothers in our lives this Mother’s Day, let’s take a special look at nutrition for moms-to-be.
Overall Dietary Pattern is Key. “From a nutrition standpoint, the most important thing to do when preparing for pregnancy and during pregnancy is to focus on an overall well-balanced diet,” says ChenChen H. Sun, MD, an obstetrician at Tufts Medical Center and assistant professor at Tufts University School of Medicine. What a mother eats during pregnancy not only nourishes her, it is also critical for the growth and development of the baby—and has the potential to affect health outcomes for both mother and child in years to come—so making healthy dietary choices is very important. Women who are pregnant or lactating need extra calories and nutrients. Just how many extra calories is determined by a number of factors, including pre-pregnancy weight and how much weight changes during pregnancy, so women should talk to their healthcare provider about calorie needs.
Make Healthy Choices: Consume a healthy dietary pattern that includes fruits, vegetables, legumes, nuts, seeds, whole grains, seafood two-to-three times a week, lean meats, poultry, and three servings of dairy a day.
Take a Prenatal Vitamin: Some nutrient needs increase in pregnancy, and dietary intake may not be enough to meet them.
Limit Mercury: Avoid high-mercury fish, like shark, swordfish, and king mackerel (see Resources for more information).
Avoid Dangerous Choices: Avoid alcohol, raw or undercooked animal proteins, and unpasteurized juice, milk, and cheeses, and limit caffeine intake to one to two caffeinated beverages a day or less.
It may be tempting to use pregnancy as an excuse to eat whatever you want. It is far better, for both mom and baby, to meet increased calorie needs with nutritious foods and beverages. Seventy percent of pregnant woman exceed the recommended intake for added sugars; and 88 percent exceed the recommended intake of sodium. The 2020-2025 Dietary Guidelines for Americans (DGAs) recommend women stick to nutrient-dense choices (those that provide vitamins, minerals, and other health-promoting components and have little added sugars, saturated fat, and sodium). This means plenty of unprocessed or minimally processed vegetables, fruits, whole grains, seafood, eggs, beans, peas, lentils, nuts and seeds, fat-free and low-fat dairy products, fish, and lean meats and poultry—prepared with no or little added sugars and sodium.
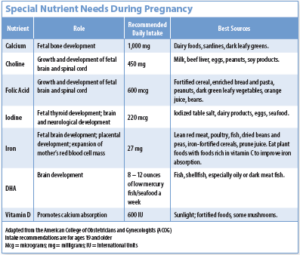
Nutrients of Concern. “There are certain key nutrients that are important for pregnant women and women of childbearing age,” says Sun. Proper nutrition supports the health of the mother and her child, is essential to the development of the fetus’ brain and body, and decreases risk for certain birth defects.
In addition to making healthy food and beverage choices, the American College of Obstetricians and Gynecologists recommends taking a prenatal vitamin daily to ensure adequate intake of important nutrients like the following:
- Calcium: “Calcium, along with vitamin D to improve calcium absorption, is important, especially in later pregnancy when the fetal skeleton is forming,” says Sun.
- Choline: Choline, a nutrient our bodies make that is also found in many foods, supports the growth and development of the child’s brain and spinal cord. A healthy dietary pattern that meets recommended intakes for dairy (three cup-equivalent servings a day) and protein—0.8 grams (g) per kilogram body weight or 0.36 g per pound)—especially from eggs, meats, and seafood, but also beans, peas, and lentils–can help meet choline needs.
- Folate/Folic Acid: Women need more folate during pregnancy and lactation than during all other stages of life. “Folate plays a crucial role in the cell replication necessary for organ development,” says Sun. “Folate deficiency can cause defects in the neural tube that becomes the brain and spinal cord. These neural tube defects can result in congenital conditions such as spina bifida.”
- Iodine: “Iodine is important for fetal thyroid development,” says Sun. Iodized table salt is a prime source of this nutrient in the U.S. diet. While increasing salt intake is strongly discouraged, women who use un-iodized sea salt may want to consider switching to iodized salt during pregnancy.
- Iron: “Women of childbearing age are a common population for iron deficiency,” says Sun. “Iron is important for fetal brain development, placental development, and accommodation for the expansion of maternal red blood cell mass that occurs during pregnancy.” The iron in plant foods is not absorbed as well as the iron in animal foods. Consume plant foods with a source of vitamin C (like red peppers, strawberries, or citrus) to improve iron absorption.
- Omega-3’s: A baby’s growing brain is mostly built from fatty acids, and the top fatty acid building block is DHA—the long-chain omega-3 found in fish and shellfish. DHA is critical for optimal development of a fetus’ brain and eyes, especially during the last trimester (three months) of pregnancy and the first two years of life, when the brain continues to develop. “Extensive research shows that women who eat more fish have babies with better brain development in childhood,” says Dariush Mozaffarian, MD, dean of the Friedman School and editor-in-chief of Tufts Health & Nutrition Letter. At least two servings of fish or shellfish per week (eight to 12 ounces) is recommended (see below for more information on seafood intake).
Foods to Watch Out For. A few foods require special attention during
pregnancy:
- Some Seafood: As described above, fish is a great source of DHA. Fish and shellfish intake by pregnant women is therefore recommended, due to the importance of DHA in brain development. But fish can also contain methylmercury, which can be harmful to the developing brain. Fortunately, the great majority of fish and shellfish are considered safe to eat (see Resources for more information). Seafood that tends to be high in mercury, such as shark, swordfish, orange roughy, tilefish, and king mackerel, should be avoided during pregnancy, and canned albacore (white) tuna should be limited to six ounces a week. But don’t let fear of these few species steer you away from other fish!
- Alcohol: The science is clear: women who are pregnant should not drink beverages

It is important for pregnant women to avoid alcohol, along with raw meats/seafood and unpasteurized milk, juice, and soft cheeses.
Image © Luca Piccini Basile | Getty Imagescontaining alcohol during pregnancy. Unfortunately, about one in 10 pregnant U.S. women surveyed reported consuming alcohol during the past month, with an average intake of two or more drinks on days that alcohol is consumed.
- Caffeine: Caffeine is not expressly prohibited during pregnancy, but women who are pregnant or could become pregnant should consult their healthcare provider for advice. “Limited research makes this a very controversial subject,” says Sun. “Generally, limiting caffeine intake to 200 to 300 milligrams (mg) of caffeine a day is recommended. I generally advise my patients that having one or two cups of coffee or other caffeinated beverages a day is okay.” Caffeine is also found in tea (except herbal teas), matcha, and many sodas, and in smaller amounts in chocolate.
- Raw foods: Women who are pregnant and their unborn children are more susceptible to the effects of foodborne illnesses from bacteria or bacterial-derived toxins than the general population. Pregnant women should only eat seafood, meats, poultry, and eggs that have been cooked to recommended safe minimum internal temperatures. They also should avoid unpasteurized (raw) juice or milk, raw sprouts, or some soft cheeses made from unpasteurized milk.
A healthy dietary pattern during pregnancy, and taking prenatal vitamins as specifically recommended by a healthcare provider, helps give baby the best start in life–and is good for Mom, too.