Left unchecked, the common condition known as insulin resistance can lead to prediabetes and type 2 diabetes. Each step of the way, the risk of heart attack, stroke, and other cardiovascular problems increases. We spoke to Anastassios Pittas, MD, MS, Chief of Endocrinology at Tufts Medical Center and a professor at Tufts University School of Medicine, to learn more about insulin resistance and how to prevent or reverse it.
HNL: What is insulin resistance?
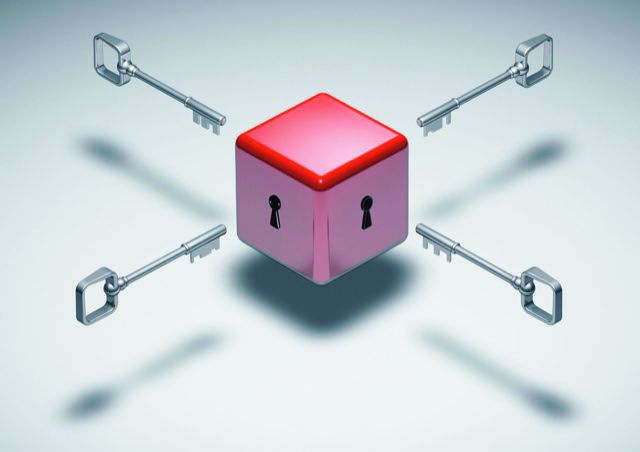
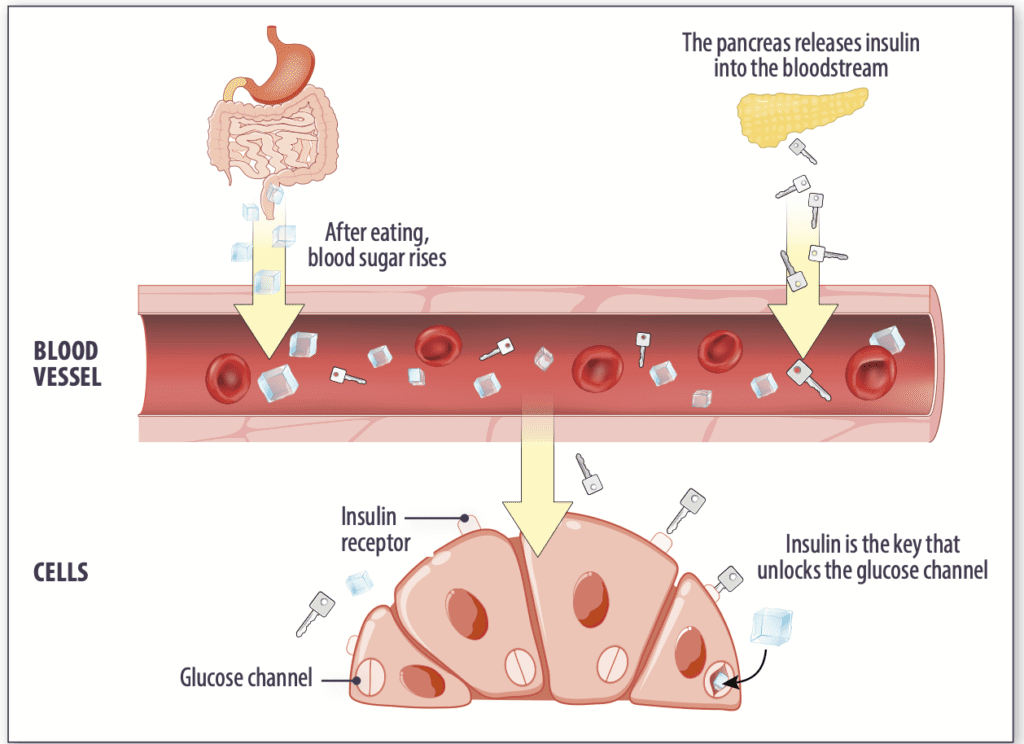
Dr. Pittas: First, let’s look at insulin and what it does. Insulin is a hormone that controls how we use and conserve energy, both when we eat and between meals. The preferred energy source for the body is the sugar glucose, and insulin plays an essential role in controlling blood glucose levels. To do this, insulin is involved in the metabolism of carbohydrates, proteins, and fats, but the most important thing to know about insulin is that it acts as a key to getting glucose into cells.
Sometimes, cells become less responsive to insulin—think of it as the key having trouble opening the lock. We refer to this as insulin resistance.
HNL: What happens if those “locks” become resistant to insulin?
Dr. Pittas: First, the beta cells of the pancreas make more insulin to push the doors harder (to continue the analogy). Eventually, the overworked beta cells can stop working, and the individual will need insulin injections to meet the body’s need for insulin.
A more immediate consequence of insulin resistance is high blood sugar. Here’s why: With insulin resistance, some glucose can’t get into the tissues. It remains in the bloodstream, leading to high blood sugar levels.
HNL: What are the possible health impacts of insulin resistance?
Dr. Pittas: Elevated glucose and insulin levels in the blood contribute to the risk of developing vascular problems (issues with blood vessels). Years of high blood sugar levels can result in permanent nerve damage, loss of vision, and kidney failure. High blood sugar also contributes to the build-up of atherosclerotic plaque in artery walls. This increases the risk of heart attack, stroke, peripheral artery disease, and dementia.
HNL: What causes insulin resistance?
Dr. Pittas: As with most conditions, it’s typically a combination of environmental factors and genetics. The most common cause of insulin resistance is excess adipose tissue—in short, weight gain. Excess adipose tissue by itself can cause insulin resistance. Additionally, if excess fat builds up in the liver and muscle, those tissues will not respond as well to insulin. There does seem to be a genetic component here, as some people are overweight or have obesity and don’t develop insulin resistance.
Studies have found an association between high triglyceride levels in the blood and insulin resistance, even in people without high blood glucose levels. Certain medications (including steroids and some HIV medications) can also cause insulin resistance. Some people have severe insulin resistance because of a genetic mutation, but this is relatively rare.
 HNL: How do we know if we have insulin resistance?
HNL: How do we know if we have insulin resistance?
Dr. Pittas: Until it progresses to type 2 diabetes, insulin resistance has no symptoms. We don’t measure insulin resistance directly. Instead, we look for the changes it causes, like high blood sugar and/or triglyceride levels. Simple blood tests that measure fasting plasma glucose, hemoglobin A1c (a measure of your average blood glucose levels over the past three months), and blood triglyceride levels help tell us if your cells are becoming resistant to the effects of insulin. A high blood insulin level is another sign of insulin resistance, but this is not commonly measured.
HNL: Is there anything we can do to help prevent insulin resistance? And can it be reversed?
Dr. Pittas: Following a healthy dietary pattern, being physically active, and losing excess weight are some key lifestyle behaviors that help prevent and decrease insulin resistance. Let’s start with diet: Refined carbohydrates (primarily foods and drinks made with added sugars and white flour) are digested quickly and enter the bloodstream as glucose, spiking blood sugar levels and increasing the need for insulin. Consuming excess calories from any source increases adipose tissue (body fat), contributing to insulin resistance.
Foods naturally high in fiber (like fruits, vegetables, whole grains, and legumes) take longer to digest, so blood sugar and insulin levels stay even. Insulin resistance is associated with a higher risk for cardiovascular problems. Choosing these foods—along with lean proteins, fat-free or low-fat dairy, and healthy unsaturated fats—is good for preventing insulin resistance and also essential for heart health. In addition, shifting to a healthy dietary pattern can help you lose excess weight.
Losing excess body fat is the most powerful approach for preventing or reversing insulin resistance and progression toward developing type 2 diabetes. You don’t need to get down to some magic number. According to data from the Centers for Disease Control and Prevention, participants in a Diabetes Prevention Program who lost five to seven percent of their body weight (and added 150 minutes of physical activity a week) cut their risk of developing type 2 diabetes by sixty percent. Additional weight loss leads to higher insulin sensitivity.
➧ Lose Some Extra Weight. Excess body weight is the key contributor to developing insulin resistance. If you are overweight or have obesity, any weight loss is helpful. ➧ Be Active. Getting your body moving for at least 30 minutes every other day contributes to lowering your blood glucose levels. ➧ Go for Natural Fiber. Consuming naturally fiber-rich fruits, vegetables, whole grains, nuts, seeds, and legumes helps keep blood glucose and insulin levels even. ➧ Limit Refined Carbs. Added sugars and refined carbohydrates like white flour and rice spike blood sugar and contribute to high blood triglyceride levels. (The fiber in unrefined—whole—carbs makes them a healthy choice.)
Physical activity can help control blood sugar even if it does not lead to weight loss. Being active moves glucose from the bloodstream into tissues without insulin. Physical activity does not improve insulin sensitivity but it does lower blood sugar levels, so the pancreas doesn’t need to produce as much insulin. The effect of exercise lasts 12 to 24 hours, so aim to engage in 30 minutes of activity or more at least every other day.