FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) are a group of sugars and fibers that serve as beneficial prebiotics, feeding the gut microbes that are important to many facets of health. Most people have no problem consuming as many high FODMAP foods as they want. Unfortunately, some people are sensitive to FODMAPs and may need to adjust their diets in order to reduce gastrointestinal symptoms.
What are FODMAPs? “FODMAPs are groups of small chain carbohydrates that are commonly poorly absorbed in the small intestine,” says Alicia Romano, MS, RD, LDN, CNSC, a Registered Dietitian/Nutritionist at the Frances Stern Nutrition Center at Tufts Medical Center. (See What Does “FODMAP” Stand For?” below).
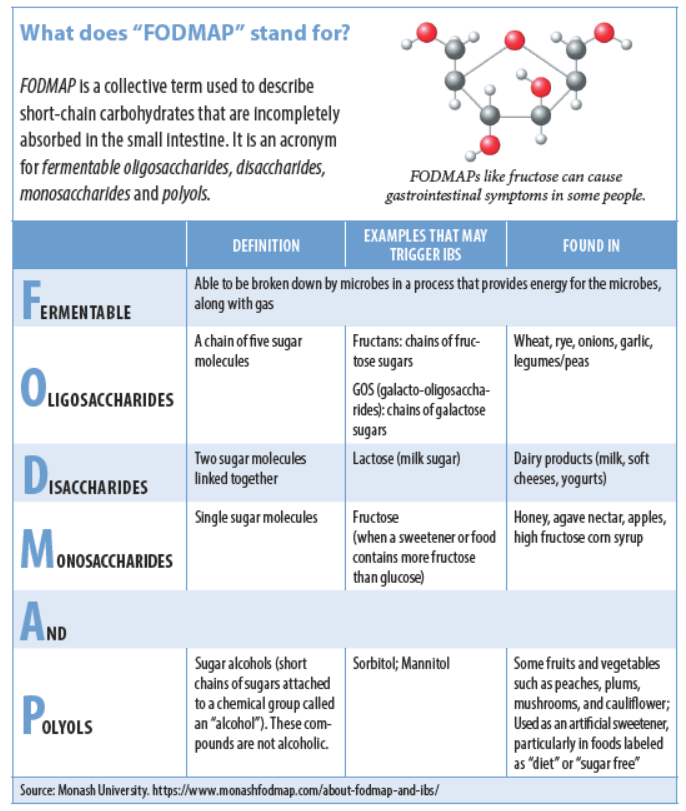
FODMAPs are found naturally in nearly all food groups. “They are in many foods that are quite common in our diet, including milk, wheat, garlic, onion, apples, watermelon, pears, honey, agave, cauliflower, and mushrooms,” says Romano. The presence or absence of FODMAPs says nothing about the nutritional value of a food (high-FODMAP asparagus and low-FODMAP green beans are both nutritious). Additionally, it’s impossible to guess the FODMAP content of a food just by looking at it or tasting it. FODMAP content varies widely within food groups. For example, apples are a high FODMAP food, and grapes are a low FODMAP food; honey is high in FODMAPs, and maple syrup is low.
Gut Check: “In those with a sensitive gastrointestinal tract, these poorly absorbed carbohydrates may lead to a cascade of unpleasant GI symptoms,” says Romano. “Unabsorbed FODMAPs in the small intestine attract water into the gut, stretching it. In patients with quick transit, this may contribute to diarrhea. The malabsorbed carbohydrates also provide a quick fuel source for gut microbiota; the gut microbes ‘feast’ off these poorly absorbed carbohydrates, leading to excess fermentation, gas, and potentially constipation. Patients with a diagnosis of irritable bowel syndrome (IBS) in particular may be FODMAP sensitive.”
Symptoms of IBS may be helped by an expert-guided low FODMAP diet.
IBS is the most common disease diagnosed by gastroenterologists in the U.S., and one of the most common disorders seen by primary care physicians. The American College of Gastroenterology (ACG) estimates that 10 to 15 percent of the adult population in the U.S. suffer from symptoms of IBS, although only five to seven percent of adults have been diagnosed with the disease. “There are a number of GI symptoms that patients may experience related to their IBS diagnosis, including bloating, gas, changes in bowel habits (diarrhea, constipation or a combination of the two), and abdominal discomfort,” says Romano. “These GI symptoms also overlap with a number of other gastrointestinal conditions, including Celiac disease, inflammatory bowel disease, heartburn, and gastro-esophageal reflux. I recommend working with your primary care physician or your gastroenterologist to obtain a proper workup and diagnosis of your GI symptoms to yield the most appropriate treatment. People should never self-diagnose or self-treat.”
Low FODMAP Diet Plan: “The low FODMAP nutritional approach was created by Australian researchers at Monash University, and continues to be studied and updated,” says Romano. There is no diagnostic test for FODMAP sensitivity. Once other digestive issues and diseases have been ruled out by a gastroenterologist, a referral may be made to a Registered Dietitian (RD) to begin a FODMAP elimination diet.
“This diet has three phases: elimination, reintroduction, and individualization,” says Romano. “The elimination phase lasts two to six weeks. If you have experienced symptomatic improvement, your RD will guide you through the next phases of the diet, including reintroduction of FODMAP food groups and then individualization to the most liberal diet possible.”
Proceed with Caution: Entirely FODMAP-free diets are not meant to be followed long-term, and they can lead to nutrient deficiencies. Foods must be added back in to liberalize the diet. “This diet has many nuances and can be tricky to follow without guidance,” says Romano. “For some patients, a low FODMAP diet may not be appropriate.”
FODMAPs are beneficial carbohydrates and intake should not be reduced unless one has Irritable Bowel Syndrome and is under medical guidance.
- See your primary care physician or a gastroenterologist if you experience unexplained intestinal distress.
- Do not undertake a low FODMAP diet without the guidance of a nutrition professional such as a Registered Dietitian
- Do not attempt long-term exclusion of FODMAPs, as this can lead to nutrient deficiencies and disordered eating
While it is generally accepted that a low FODMAP diet can be effective in reducing or alleviating IBS symptoms, research on the subject is somewhat limited. A 2018 review of randomized controlled trials published in the American Journal of Gastroenterology found evidence that a low FODMAP diet was effective in treating symptoms of IBS, although it graded this evidence as “very low quality.” The authors indicate this rating is a result of low study size and potential for the placebo effect, given that participants could easily tell if they were being put on a low FODMAP diet or not. Additionally, study durations were typically short.
A low FODMAP diet is generally low in dietary fiber, an important health-promoting bioactive food component. The diet is complex, can lead to low calorie intake, and may reduce concentrations of beneficial gut microbes. It also is difficult for vegans and vegetarians to adhere to and is potentially dangerous for people with diabetes and those with a history of eating disorders. While this diet is the most effective dietary intervention for IBS to date, it should not be undertaken without guidance from a nutrition professional.
“If you have been diagnosed with IBS,” says Romano, “the low FODMAP diet may play an important role in your symptom management along with other traditional medical therapies.”
Monash University
Monash University conducts laboratory analyses to understand FODMAP content of food and makes this information (and other information on IBS and FODMAPs) available online and in a free mobile phone app. The app uses a traffic light rating system to indicate whether foods are low (green), moderate (yellow), or high (red) in FODMAPs.
For more information, see MonashFODMAP.com




















This is very helpful. I have been diagnosed with IBS and this is a good explanation of the food I’m to look out for in my diet.