[Updated May 10, 2018]
DIABETES DIET: OVERVIEW
1. Maintaining good blood glucose levels is essential, and carbohydrates tend to raise blood glucose levels in diabetics.
2. Limit sugar and carbohydrates and consumption. See a complete list of carbohydrate foods below, as well as the foods you should be eating for diabetes.
3. Plan meals and snacktimes ahead, and spread them out over the course of the day for better blood sugar control.
One of the biggest challenges many people face when they find out they have diabetes is figuring out what they can eat and when. Fortunately, healthy eating when you have type 1 or type 2 diabetes (or prediabetes) isn’t substantially different from how we all should eat. Diabetes-friendly diets feature the same healthy foods – whole grains, colorful non-starchy vegetables, whole fruits, lean protein, fish, low-fat dairy, nuts and healthy fats – recommended for everyone.
“If you have prediabetes or diabetes, your meals can still be (and should be) enjoyable,” emphasizes Denise Arthurs, MS, RD, a clinical dietitian/nutritionist at the Frances Stern Nutrition Center at Tufts Medical Center. “In the past, diabetes diets were fairly rigid. Today, the guidelines of the American Diabetes Association (ADA) focus on healthful eating patterns that feature a variety of nutrient-dense foods in appropriate portion sizes to help you meet your weight goals.”
Healthy Body Weight and Diabetes:
Underlying diabetes diet guidelines is the importance of following a heart-healthy eating plan and maintaining a healthy body weight. People with diabetes have two to three times greater risk of cardiovascular disease, including heart attack and stroke, compared to people without diabetes.
To learn more, see: Healthy Fats Reduce Diabetes Risk
Modest weight loss, if you’re carrying extra weight, reduces risk of cardiovascular issues. It also can delay progression from prediabetes to type 2 diabetes. “In people with prediabetes or type 2 diabetes who are overweight or obese, losing at least 5% – and ideally 7% or more – of body weight (and sustaining that loss) can significantly improve blood sugar control,” Arthurs says. When your blood sugar is under better control, you feel better, too.
Carbohydrates and Controlling Blood Sugar:
Carbohydrate is in the spotlight in diabetes meal planning. That’s because the carbohydrate you eat is ultimately broken down and converted to glucose in the body (if not consumed directly as glucose), which raises blood sugar, also called blood glucose. In type 1 diabetes, there is a complete absence of insulin needed to lower blood sugar, while in type 2 diabetes, the body doesn’t produce enough insulin and the body’s cells aren’t responsive enough to it.
“That doesn’t mean a person should completely avoid carbohydrate-containing foods; they’re an important source of energy, essential nutrients and fiber,” Arthurs says. “But, you do need to pay attention to the amount and timing.” That requires knowing which foods contain carbs and which ones don’t (see “Carbohydrate Foods,” right).
“The carbohydrate-containing foods we encourage people with diabetes to eat are those that are the least refined or processed because they’re generally gentler on blood sugar,” Arthurs says. For example, steel-cut oats (oat kernels simply broken into a few pieces) or rolled oats are a better choice than instant oatmeal, especially if flavored and sweetened.
“However, that doesn’t mean you can never eat a piece of pie or a serving of ice cream,” Arthurs says. “Those foods can fit in small portions, but they should be a treat, not everyday foods.” If you know you’re going to eat a scoop of ice cream at a birthday celebration, for example, then skip a carbohydrate-rich food you’d normally eat at that meal, such as the dinner roll or mashed potatoes. That can help prevent a big rise in your blood sugar.
Blood Sugar Goals for Diabetics
“If people with diabetes check their blood sugar with a glucose meter, it helps them determine their body’s individual response to what they eat,” Arthurs says.
The American Diabetes Association recommends the following general blood sugar goals in diabetes, but your health care provider may modify these based on your individual needs.
When you wake up and before meals: 80 to 130 mg/dL
2 hours after start of a meal: Less than 180 mg/dL
Best Foods for Diabetes:
As you think about a diabetes diet, Arthurs encourages you to first look at how you normally eat. Are some of your meals mainly carbohydrate-rich foods and little else? Have you aimed for a balance of different types of food at meals – for example, non-starchy vegetables, a whole grain, lean protein and a small amount of heart-healthy fat?
“Controlled trials show that eating more healthy fats, in particular polyunsaturated fats from plants and plant oils (such as soybean, corn and other liquid vegetable oils), leads to better blood sugar control and improved insulin sensitivity,” says Dariush Mozaffarian, MD, DrPH, dean of Tufts’ Friedman School. “Also consider probiotic-rich foods like yogurt. Emerging science suggests these may also support blood sugar control, perhaps through maintaining a healthy gut microbiota (good bacteria), but more research is needed.” Of course, remember that if you increase one component in your eating plan, decrease another so your total caloric intake doesn’t exceed your needs.
Don’t overlook beverages in your assessment. Are you drinking empty-calorie, sugary carbs, such as soda? The ADA advises avoiding sugar-sweetened drinks to help with weight control and reduce risk of cardiovascular disease and fatty liver disease (also a common companion to type 2 diabetes). Even drinking 100% fruit juice can make it more challenging to control blood sugar and fatty liver risk. A better choice is whole fruit, which comes in nature’s own portion-controlled packages and with fiber to slow digestion.
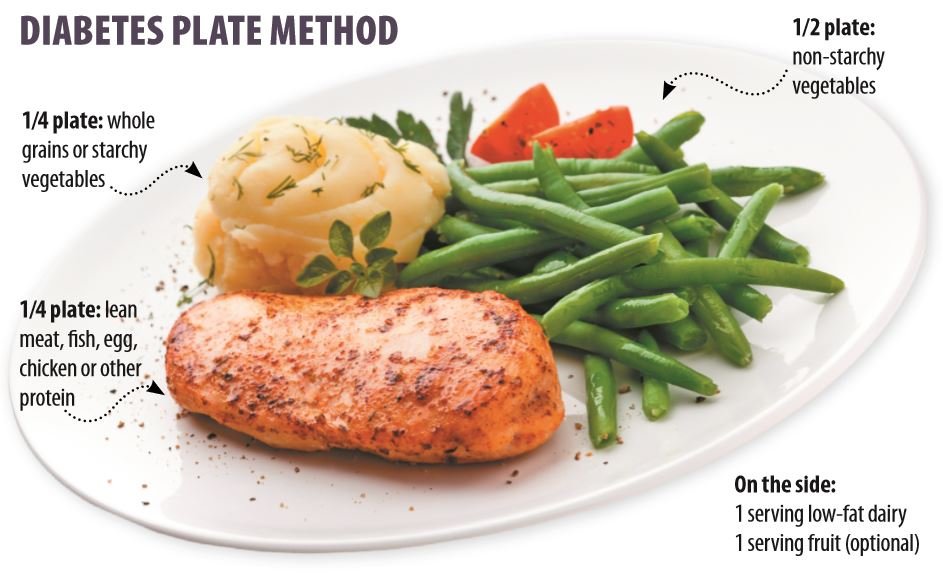
One approach that can help you put dietary recommendations together is the diabetes plate method (pictured, above). If you already useTufts MyPlate for Older Adults, planning what to put on your plate in diabetes is not very different. The main change is that fruit is moved off the plate as an optional dessert, as your meal plan allows, and its place on the plate is filled by non-starchy vegetables. This approach makes it easy to plan healthful meals and not over-do meat and starchy foods.
In addition to types and amounts of carbohydrates, the evidence and guidelines, such as from theAmerican Diabetes Association, support a focus on overall healthier food choices. The diabetes plate method easily accommodates healthy eating patterns such as the Mediterranean-style diet, which is rich in produce and healthy fats and proteins, particularly minimally processed, bioactive foods (those rich in phytochemicals and other trace beneficial compounds) like non-starchy vegetables, fruits, nuts, legumes (beans) and fish.
Not only has the Mediterranean diet been shown to reduce risk of type 2 diabetes, but a recent review of clinical trials published in theEuropean Journal of Clinical Nutritionfound the diet was associated with improved blood sugar control, body weight, blood pressure, blood cholesterol and triglycerides, compared to control diets (which covered a range, including low-fat, low-carb to high-carb or simply usual dietary habits) in people with type 2 diabetes.
Counting Carbohydrates and Diabetes:
If you’re ready to take diabetes meal planning to the next level, you can count your carbohydrate grams or carbohydrate servings, sometimes called carb counting, in addition to planning a balanced plate with nutrient-rich foods. Look up the carb grams in foods by using nutrition labels, recipe nutrition information, books, restaurant websites, smartphone apps and online food databases such as from the USDA or the ADA.
In diabetes meal planning, one carbohydrate “serving” or “choice” has an average of 15 grams carbohydrate. So, if you eat an English muffin that has 30 grams carb, it counts as 2 carb servings.
How many carb servings should you eat at a meal or snack? Use “Carb Counting Budget,” right, as a general guide, but this is best determined with the help of a registered dietitian or diabetes educator while considering your body size, activity level and weight goals (and insulin regimen, if applicable). These experts can also help you master carb counting.
What about going low carb? “Both doctors and the public are increasingly interested in very-low- carbohydrate diets (for instance, 10 to 15% or less of calories from carbs),” Mozaffarian says. “Assuming your overall diet is high in minimally-processed, bioactive foods and healthy fats and proteins, a very-low-carb dietary pattern could be considered together with your doctor.”
The Carb-Counting Budget for Diabetics
General guidelines for carbohydrate servings:
Women:3-4 carb servings per meal; 1 carb serving per snack
Men:4-5 carb servings per meal; 1 or 2 carb servings per snack
To learn more, see:Choose the Right Carbs to Help Control Your Diabetes Risk
Carbohydrate Foods to Limit
– Grain foods, such as bread, baked goods, cereal, crackers, pancakes, rice, tortillas and pasta
– Starchy vegetables and legumes (beans), such as white potatoes, sweet potatoes, corn, parsnips, winter squash, peas and lentils
– Non-starchy vegetables (minimal carbs), such as asparagus, broccoli, carrots, cauliflower, cucumber, green beans and leafy greens
– Fruit and fruit juice
– Milk, milk substitutes and yogurt
– Seeds, nuts and unsweetened nut or seed butters (minimal carbs)
– Sugary beverages, such as regular soda, sports drinks and energy drinks
– Some condiments, such as jelly, barbecue sauce, ketchup and many salad dressings
– Sweeteners, such as sugar, honey, concentrated fruit juice, maple syrup and corn syrup
– Sweets, such as ice cream, cake and candy
Foods that contain little to no carbohydrate include plain meat, poultry, fish, eggs, cheese, olives, buttery spreads, sour cream, mayonnaise, cooking oils and shortening. Check labels to be sure.
Diabetes Meal Planning:
Keep regular eating times distributed across the day (and coordinated with diabetes medication and insulin regimens, as applicable). Whether or not you eat snacks is up to you and will depend on what time you eat meals and should be aligned with your weight goals. If you eat breakfast at 9 a.m. and lunch at noon, you probably don’t need a morning snack. But if you don’t eat again until 6 p.m., a mid-afternoon snack may help control hunger and blood sugar.
“Blood sugar rises after meals (and snacks), so spacing out eating times gives blood sugar a chance to come back down between meals,” Arthurs says. “It’s also important not to eat too much at a time. It would be really hard for people with diabetes to control their blood sugar levels if they ate one big meal a day and didn’t eat at any other time. Blood sugar would be really high after the large meal.” Over the long run, high blood sugar can increase risk of diabetes-related damage to blood vessels, such as in the cardiovascular system, eyes and kidneys.
Don’t skip breakfast, as eating your morning meal may be particularly helpful for blood sugar control. In research, skipping breakfast has been consistently associated with higher A1C (a measure of average blood sugar over about 3 months) in type 2 diabetes.
So, whether you’re new to managing diabetes or have been working on it for a while, there’s a lot you can do from a dietary standpoint to help you live well with diabetes. You don’t have to master diabetes guidelines overnight, and many health practitioners are available to help.
To learn more:




















Great Post! Thanks for sharing this with us.
Wonderful content as always. I love how you talk about the projects and topics in detail. Keep the articles coming.