In estimated 10 million Americans have osteoporosis, a bone disease that occurs when the body loses calcium from bone faster than it builds new bone, leading to low bone density. This condition increases the risk of a broken bone. Such fractures happen in about half of women and up to one quarter of men over age 50 who have osteoporosis.
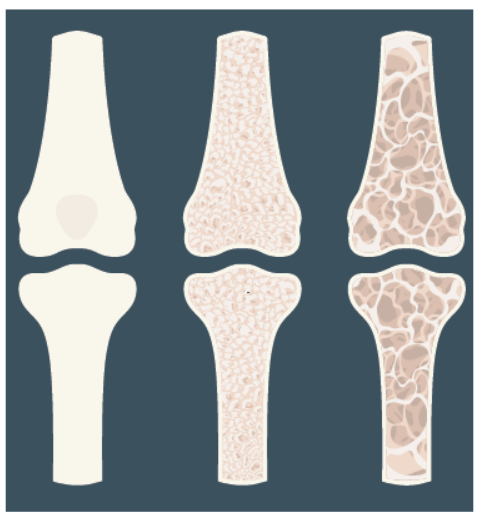
Know Your Risk. Osteoporosis literally means porous bone. “Under a microscope, healthy bone looks like a honeycomb, says Andrea J. Singer, MD, chief medical officer of the National Osteoporosis Foundation. “With osteoporosis, the spaces in the honeycomb become larger.” The bones become weak and more likely to break.
Risk for osteoporosis increases with age (especially after age 65). While this disease can affect men and women of all races, “women are more at risk than men because they tend to have smaller, thinner bones to begin with,” says Singer. “White women and women of Asian descent are at higher risk, and risk for all women increases when levels of estrogen decrease after menopause.” Other risk factors include a family history of osteoporosis or hip fracture, smoking, alcohol intake, inactivity, vitamin D deficiency, and certain medical conditions (including diabetes and rheumatoid arthritis) and medications (such as glucocorticoids).
A bone mineral density test is used to determine if you are at risk for or have osteoporosis. This test uses X-rays to determine the mineral density of your bones. The National Osteoporosis Foundation recommends the following groups get a bone density test:
- women age 65 or older;
- men age 70 or older;
- postmenopausal women under age 65 with risk factors; and
- men age 50 to 69 with risk factors.
A fracture later in life should also trigger a test. “If you are a postmenopausal woman or a man age 50 or older and have broken a bone (excluding fingers, toes, face, or skull), you should definitely speak to your healthcare provider about getting a bone density test,” suggests Singer. The results of the initial test will determine the need for and timing of future screenings.
Take action to prevent osteoporosis:
- Nourish your Body. Follow a healthy dietary pattern that includes calcium and viatmin D from foods like dairy or fortified dairy substitutes and fatty fish. Fruits and vegetables also contain nutrients important to bone health.
- Move it! Engage in regular physical activity, including weight bearing, muscle strengthening, and balance exercises.
- Cut out vices. Do not smoke and limit alcohol use.
- Know your risk. Postmenopausal women are more at risk than men. Age over 65, family history, smoking, excessive alcohol intake, inactivity, and vitamin D deficiency are common risk factors.
- Get tested. Discuss whether you should get a bone density scan with your healthcare provider.
What to Do. Being physically active and consuming a healthy dietary pattern are critical steps in helping prevent calcium loss from your bones. Dairy products are the main source of calcium in the American diet. If you do not eat dairy, consider dairy substitutes fortified with this mineral. Fish with bones (like sardines, anchovies, and some canned salmon) contain calcium, and some plant foods, like leafy greens and almonds, contain smaller amounts. Check labels of processed foods and beverages, such as orange juice, to see if they are fortified with calcium. The Recommended Daily Allowance (RDA) for calcium is 1,000 milligrams (mg) daily for women age 50 and younger and men age 70 and younger, and 1,200 mg daily for older women and men. See page 4 for information on how to get adequate dietary vitamin D.
Magnesium, potassium, vitamin C, and vitamin K are also important for bone health. The fruits and vegetables in your diet supply plenty of these nutrients. “If you eat a healthy dietary pattern with plenty of dairy, fish, fruits, and vegetables, you should get enough of the nutrients you need,” says Singer. “If you’re not getting the recommended amount from food alone, however, you may need to complement your diet by taking supplements.”
If you are not deficient, there is currently no clear evidence that supplements are help
ful. In 2018, the U.S. Preventive Services Task Force concluded that daily supplementation with 400 IU or less of vitamin D combined with 1000 mg or less of calcium did not help lower the incidence of fractures in postmenopausal women. (Note that there was not enough information to determine the effects of higher doses in this population, or the effects of supplementation on fracture risk in men and premenopausal women.)
“It’s important that everyone take simple steps to help protect their bones,” Singer says, “because bone health is critical to safeguarding your ability to live an active, independent life as you age.”
























It seems that a high percentage of people are borderline deficient in Vit D and that a substantial D3 supplementation is healthy and wise….. along with supplemental K-2. ( All supplements are NOT a waste of money )