IMAGE © THINKSTOCK
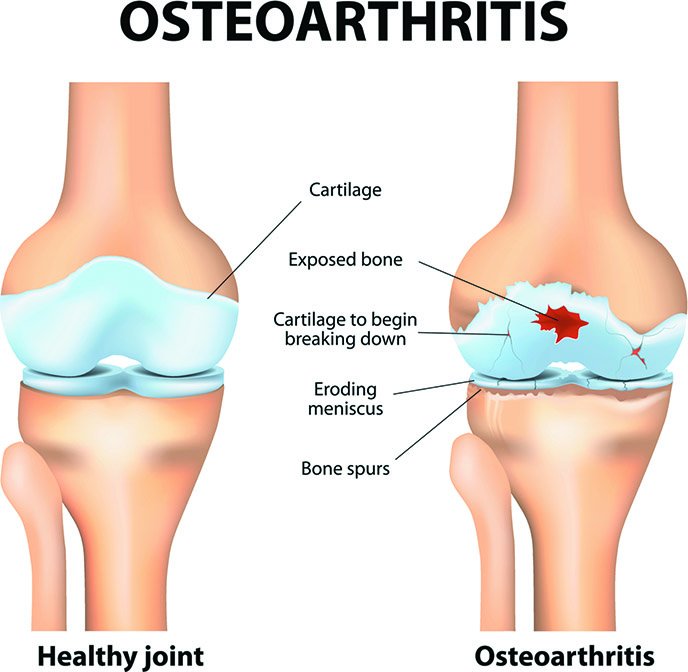
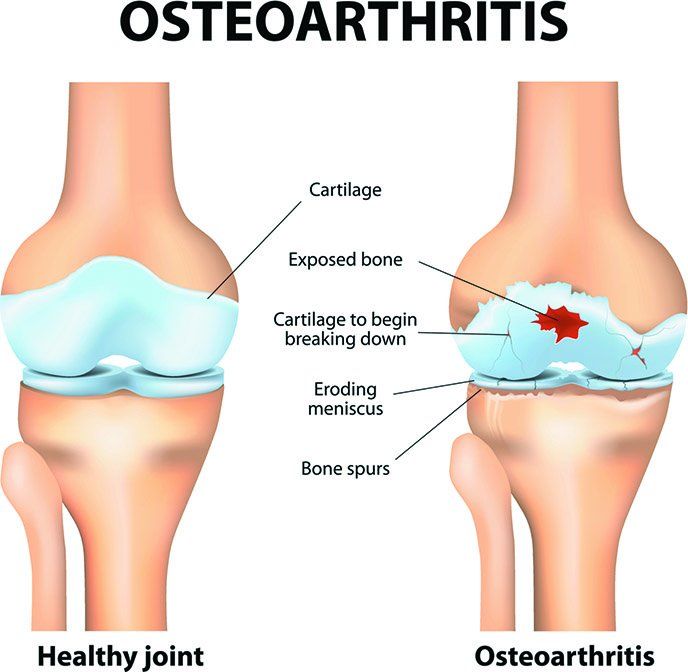
Here’s another reason to make sure you’re getting enough vitamin D: A recent Tufts study suggests that vitamin D deficiency may be associated with greater risk of osteoarthritis (OA) of the knee. Compared to those with adequate blood levels of vitamin D, participants low in the “sunshine vitamin” were twice as likely to experience worsening of knee osteoarthritis. Those deficient in vitamin D as well as a hormone involved in metabolizing the vitamin were at triple the risk.
“Vitamin D influences cartilage, bone and particularly muscle, all of which have important roles in the progression of knee osteoarthritis,” explains Fang Fang Zhang, PhD, an epidemiologist and assistant professor at Tufts’ Friedman School who was lead author of the study. “Our results suggest that individuals deficient in vitamin D have an increased risk of knee osteoarthritis progression.”
ENOUGH, NOT EXTRA: Results of previous studies of vitamin D and knee OA have been mixed. Some observational studies have seen an association between low levels and increased risk, but two clinical trials of vitamin D supplementation found only a small benefit or none at all.
The new study, published in the Journal of Nutrition, looked at data on 418 participants in the Osteoarthritis Initiative, the most comprehensive study of knee OA in those at risk. Participants had been tested for blood levels of vitamin D and parathyroid hormone (PTH). Radiographs were used to assess knee OA progression over four years.
An association between low vitamin D status and OA risk was seen only in participants identified as deficient in vitamin D, using the Institute of Medicine’s standard of 15 nanograms per milliliter (ng/ml) of blood serum. (Other experts use a higher cutoff for vitamin D deficiency.) Zhang and colleagues speculated there might be a “threshold effect,” in which risk is reduced by achieving adequate vitamin D levels—but more vitamin D does not confer extra protection.
In fact, study participants who self-reported greater dietary intake and supplementation of vitamin D were not at significantly lower risk of OA progression. That supports the idea that getting enough is important, but there’s no anti-arthritis benefit from more.
CAUSES AND EFFECTS: As an observational study, the research was not designed to prove cause and effect. It could be that some other factor affects both vitamin D status and OA progression.
In 2014, another observational study reported that four out of five participants in Greece—a sunny Mediterranean country—with knee or hip OA were also deficient in vitamin D (defined as below 20 ng/ml). This unexpected finding led those researchers to suggest considering “other predisposing factors.” For example, vitamin D deficiency has been associated with obesity, which contributes to the progression of osteoarthritis. In the recent Tufts study, participants with a higher BMI were more likely to be low in vitamin D.
In any case, getting adequate vitamin D is proven to be important in keeping your bones strong and preventing osteoporosis. If avoiding low vitamin D status also gives you an edge against osteoarthritis, consider that a bonus.
The Institute of Medicine recommends that people ages 4 through 70 get at least 600 IU daily of vitamin D. For individuals over age 70, the recommendation rises to 800 IU. Dietary sources of vitamin D include:
– Swordfish
– Salmon
– Canned tuna
– Fortified orange juice
– Fortified milk and other dairy products
– Sardines
– Beef liver
– Eggs
– Fortified cereals