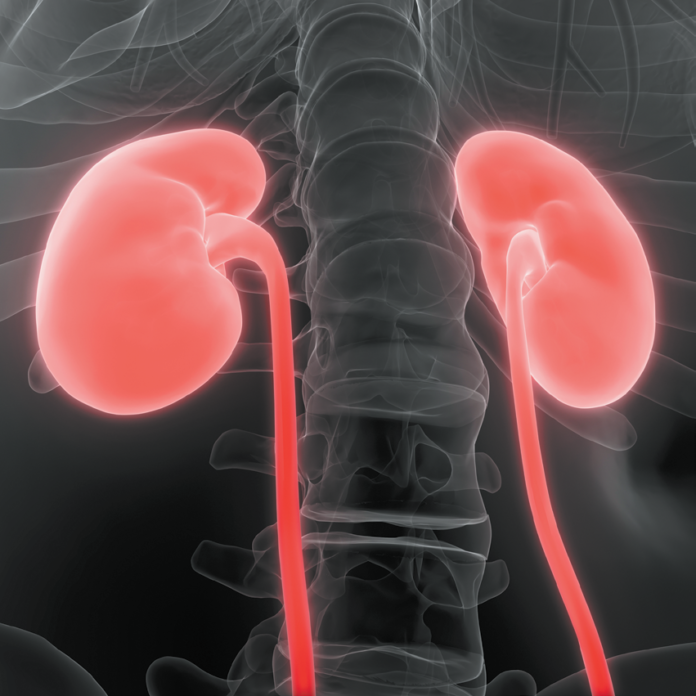
It is estimated that one in ten people will have a kidney stone some time in their lives. Each year more than half a million people visit emergency departments to get treatment for kidney stone pain or intervention to remove larger stones. The prevalence of kidney stones in the U.S. has more than doubled since the 1970s.
Many Factors, Many Types: A wide variety of factors contribute to the formation of kidney stones, including genetics; obesity; malabsorption; history of gastric bypass; health conditions including diabetes, hyperparathyroidism, and gout; certain medications; gut microbiome composition, vitamin C supplements of over 1,000 milligrams (mg) a day; and low calcium intake. Each of these factors can increase the concentration of certain elements or compounds in the urine, and crystals may begin to form. The crystals attract other elements and form a solid mass. The most common kidney stones in the U.S. are calcium-containing stones (mainly calcium oxalate with some calcium phosphate). Uric acid stones are the second most common, while other types are rarer. “Within these categories, the composition of stones varies quiet a lot, and most stones we analyze are actually a combination of components,” says Kristina Penniston, PhD, RD, senior scientist in the department of urology at University of Wisconsin Medical School and clinical nutritionist for the University of Wisconsin Hospital Metabolic Stone Clinic. “In fact, it’s possible no two stones are alike. For that reason, there is no one-size-fits-all stone diet.”

Diet Facts and Misconceptions: In a 2018 study, nearly one in five U.S. emergency departments surveyed recommended people presenting with kidney stones decrease their calcium intake, but this is bad advice. “Epidemiological studies show that consuming less than 500 mg of dietary calcium a day is associated with higher risk of calcium oxalate kidney stones,” says Haewook Han, PhD, RD, clinical assistant professor of nutrition at the Friedman School and a renal nutritionist at the Frances Stern Nutrition Center. The American Urological Association recommends people with calcium stones and relatively high urinary calcium consume 1,000 to 1,200 mg per day of calcium, preferably from diet (with meals), not supplements. This is the same range of dietary calcium intake recommended for all adults in the U.S.
Low oxalate diets are often suggested to prevent recurrence of stones, but this diet could actually increase risk for calcium oxalate stones. In a randomized controlled trial, a low-oxalate diet did reduce urine oxalate, but it also reduced compounds known to inhibit stone formation. “High oxalate content is actually a marker of a healthy diet,” says Penniston, “because oxalates are found in health-promoting choices like whole grains, vegetables, nuts, and seeds. The key is not to limit dietary oxalates, but to control their bioavailability. This can be done quite easily by consuming calcium-containing foods and beverages with meals. Some of the calcium will bind with oxalate and be excreted in the stool, keeping urine oxalate levels from rising.”
The most common stones tend to form in overly acidic urine. Diets that emphasize non-dairy animal proteins (meat, poultry, and fish) make urine more acidic. Vegetables and fruits (even acidic citrus fruits) actually make urine less acidic, decreasing risk for kidney stones. These foods are also critical components of a health dietary pattern.
What to Do: A healthy diet can help prevent kidney stones (unless there is a medical, genetic, or other non-dietary cause). For those who already have kidney stones, analyzing the chemical makeup of a stone (if it can be caught) and/or evaluating a 24-hour urine collection and reviewing a thorough medical history are the best ways to develop a personalized plan to prevent stones from recurring. Even if that is not possible, following a healthy diet—rich in fruits and vegetables, low in salt, with adequate calcium, plenty of unsweetened fluids, and not too much meat—is good for general health as well as kidney stone prevention. (See Take Charge! for more information)
- Get plenty of fluids from non-sweetened beverages and foods like fruit, soup, and yogurt
- Consume adequate calcium (1,000 to 1,200 mg, mostly from dietary sources like dairy products)
- Consume calcium-containing foods and beverages (like dairy products and calcium-fortified beverages and foods) with meals to reduce oxalate absorption
- Reduce sodium intake to the recommended 2,000 to 2,300 mg/day
- Avoid high doses (over 1,000 mg/day) of vitamin C supplements
- Follow a DASH-style or vegetarian diet—with a high intake of fruits and vegetables, legumes, nuts/seeds, dairy products, and whole grains
- Limit intake of non-dairy animal proteins like meat and poultry
- Attain and maintain a healthy weight
- Work with a nephrologist, urologist, or registered dietitian to individualize treatment if you have had kidney stones
- Avoid over-the-counter supplements that claim to prevent or break up stones, as none are supported by science



















Excellent
Very helpful!! Have hx of many stones and lots of the issues described.
Thanks for all the info!
I don’t understand what the recommendation “Limit intake of non-dairy animal proteins like meat and dairy” means. Vague words like “limit” aren’t helpful because they can mean different things to different people!